
A venous ulcer is a shallow skin wound that develops when the veins don’t return blood back toward the heart as they normally would. (This is venous insufficiency). These ulcers usually develop on the sides of the lower leg, above the ankle and below the calf. Venous skin ulcers, also called statis leg ulcers, heal slowly and often come back without preventative treatment.
What causes venous ulcers?
Veins have one-way valves that keep blood circulating to the heart. In venous insufficiency, the valves are damaged, and blood backs up and pools in the vein. This causes inflammation around the vein, irritating the overlying skin causing skin breakdown and ultimately ulcer formation.

What are the symptoms?
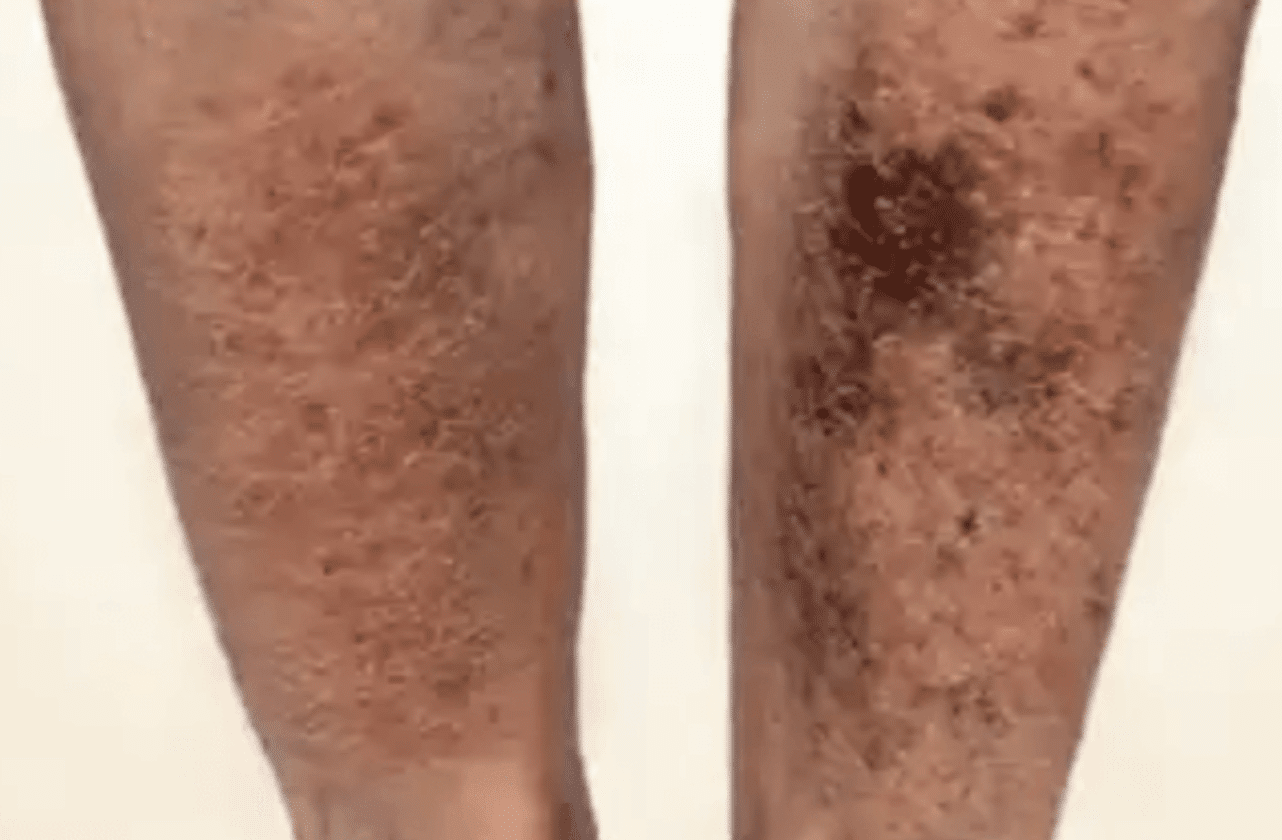
Prior to ulcer formation, the skin turns dark red or purple. Skin may also become thick, dry and itchy. Untreated, an ulcer may form and become painful. Legs may become swollen and sore. An infected wound may cause an odor, and puss may drain from the wound. The area around the wound also may be more tender and red. It’s important to call us when you first see signs of a venous ulcer, as we may be able to help prevent the ulcer from forming. And, if it is formed, seek treatment immediately; smaller and newer ulcers heal faster.
How are venous skin ulcers diagnosed?
Your doctor will ask questions about your health and will examine affected areas. They may also perform ultrasound testing. All can be done within the comfort of the office. Your doctor may use other tests to check for problems related to venous skin ulcers or to recheck the ulcer if it does not heal within a few weeks after starting treatment.
Why Choose Vein Specialists of Geneva
At Vein Specialists of Geneva, you receive personalized, compassionate care designed to heal venous ulcers and prevent recurrence. The experienced team uses state-of-the-art technology and minimally invasive treatments to restore your leg health. You are guided through every stage of care—from diagnosis and wound management to lifestyle education and prevention strategies. With a focus on comfort, safety, and long-term results, Vein Specialists of Geneva helps you achieve healthier legs and lasting relief.
FAQs About Venous Ulcers
Who Is Most at Risk for Venous Leg Ulcers?
You are more likely to develop a venous ulcer if you have varicose veins, chronic swelling, or a history of blood clots. Your risk also increases with age, obesity, limited mobility, or prolonged standing or sitting. Pregnancy, leg injuries, and a family history of vein disease can further contribute to developing ulcers. Recognizing your risk factors helps you take early steps toward prevention and timely treatment.
Can You Have Both Venous and Arterial Disease, and Does That Change Treatment?
Yes, you can have both venous and arterial disease at the same time. When both are present, treatment must be customized to safely improve blood flow. While compression therapy benefits venous ulcers, it must be adjusted carefully if arterial disease is also present. Your provider performs a thorough vascular evaluation to determine the safest and most effective treatment approach for your situation.
How Long Do Venous Ulcers Typically Take to Heal?
Healing time depends on the size and severity of the ulcer, as well as your overall health and how well you follow your treatment plan. Many ulcers start to improve within weeks, but deeper or chronic wounds can take several months to heal. Keeping your ulcer clean, using prescribed compression therapy, and maintaining healthy circulation all help speed up recovery.
How Much and How Often Should You Elevate Your Legs Each Day?
You should elevate your legs above heart level several times a day for about 30 minutes per session. This position helps reduce swelling, improve blood flow, and relieve discomfort. Regular elevation after long periods of standing or sitting can also help prevent ulcers from worsening or returning.
Can You Shower, Bathe, or Swim with a Venous Ulcer?
You can shower if you protect the wound dressing from getting wet, but you should avoid soaking in a bath or swimming until the ulcer has completely healed. Immersing the wound can increase the risk of infection and delay healing. Always follow your provider’s instructions for wound care and hygiene.
How Can You Prevent Venous Ulcers from Coming Back After Healing?
To prevent recurrence, continue wearing compression stockings as prescribed and elevate your legs regularly. Staying active through walking or calf exercises helps improve circulation. Managing your weight, avoiding extended sitting or standing, and taking care of your skin are also important steps to maintain vein health and reduce the chance of ulcers returning.
What Daily Habits Help Support Healing?
Daily movement and light exercise support healthy blood flow and help your legs heal faster. Walking, calf raises, and gentle stretching strengthen your leg muscles and assist circulation. Maintaining a balanced diet, staying hydrated, and following your wound care routine all contribute to long-term healing and prevention.
Contact our office today at (630) 425-0800 to schedule an appointment with Dr. Kern and begin your journey to healthier, pain free legs.

